By Hanna Bogen, M.S., CCC-SLP

In the part one post I introduced readers to the fundamental principles of improvisation (“improv”) and the connections between improv and social-regulation. Again, they include:
- Principle One: Be prepared
- Principle Two: Willingness (to fail spectacularly)
- Principle Three: Stay in the moment
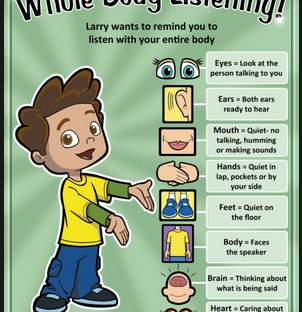
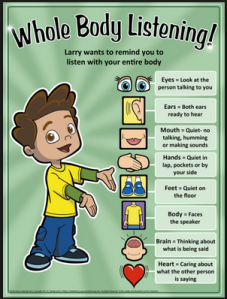
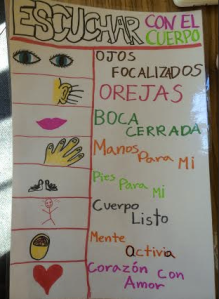
- Principle Four: Quiet down and listen
- Principle Five: Action beats inaction
- Principle Six: Be honest
- Principle Seven: Let go of your need to control
- Principle Eight: There are no mistakes
- Principle Nine: Trust
- Principle Ten: Teamwork
These principles of improv (Peter Bromberg, 2007) demonstrate the value of flexibility, perspective taking, and reciprocity in successful social interactions. This blog post will take a deeper look at three of the principles and their necessity in the world of social-regulation, specifically: willingness, stay in the moment, and “Yes, and…”
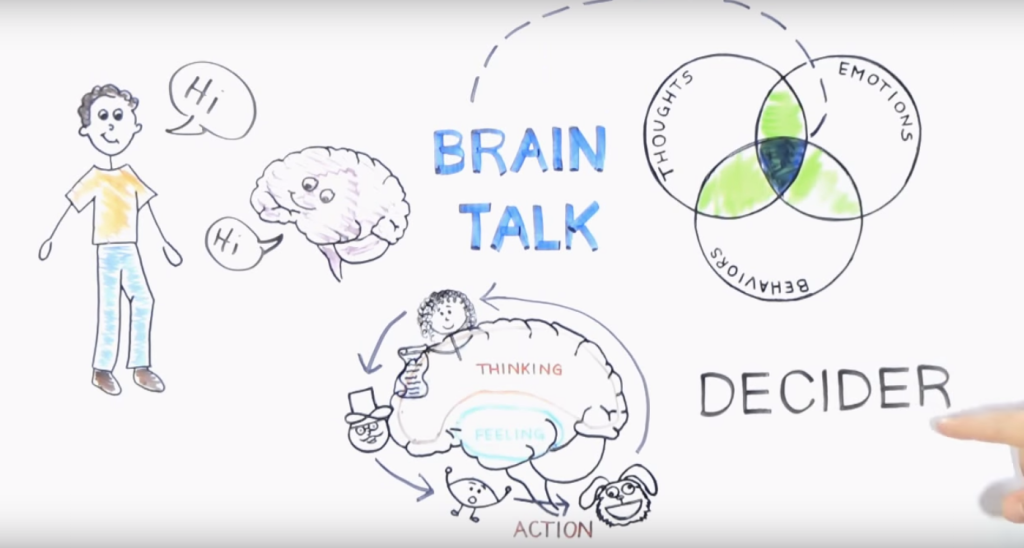
Willingness: One constant we can count on time and again is that social behaviors have consequences — others either have comfortable, positive thoughts about us or uncomfortable, negative thoughts about us based on the things we do. While the brain is inclined to stick with reliable behaviors with predictable outcomes, social situations often require us to push the comfort zone and try something new. Individuals with social-regulation challenges may struggle to shift away from predictable behaviors, even when they have socially-unexpected outcomes. Willingness to ask new questions, attempt new connections, and risk the possibility of failure is key to learning and adapting to increasingly more mature forms of communication. In improv, the structure and rules of the games offer a safe place to try new things because it is ok to make mistakes; mistakes are often celebrated with shared laughter, which builds confidence in in students. Along with this willingness to evolve is the need to reflect on one’s social experiences: “Did the interaction go as planned?” “How did the conversation partner react to the comment?” “What might I do differently next time to have a more socially-expected outcome?” Acknowledging that mistakes are inevitable in social development, and engaging in thoughtful reflection on social behaviors and their consequences, provide a context for successful social growth.
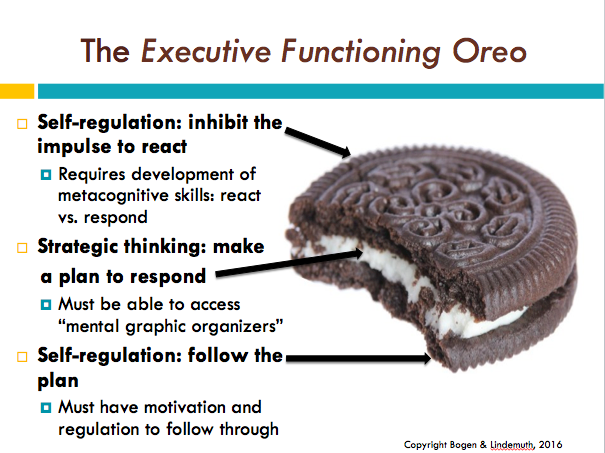
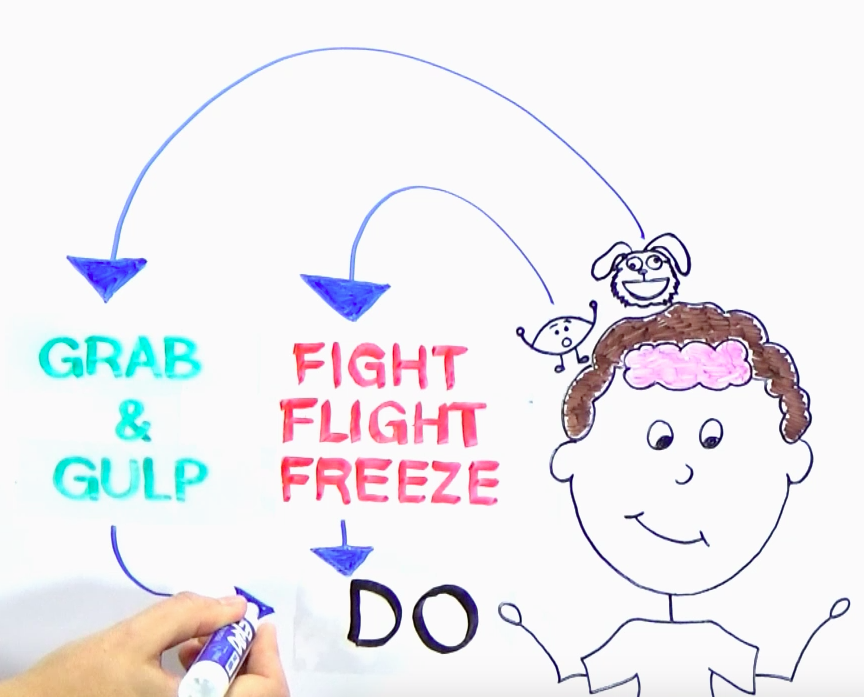
Stay in the Moment: Successful executive functioning hinges on one’s ability to engage in “mental time travel” (i.e., the ability to use foresight and hindsight to make decisions in the present moment). That being said, mindful, nonjudgmental awareness of the present moment allows individuals to make intentional decisions about how to behave at any given moment, rather than simply being carried away by impulses and emotion. The mindful practice of staying in the moment, even when that requires regularly redirecting thought and attention from the past or future to the present, strengthens our brain’s ability to “insert the pause” between stimulus and response, thus improving self-regulation skills. This “pause” represents an individual’s opportunity to decide whether (s)he wants to continue with a social behavior, or redirect to a new, more socially-expected one.
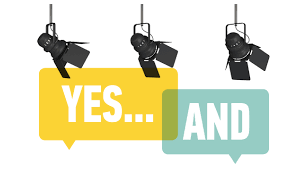
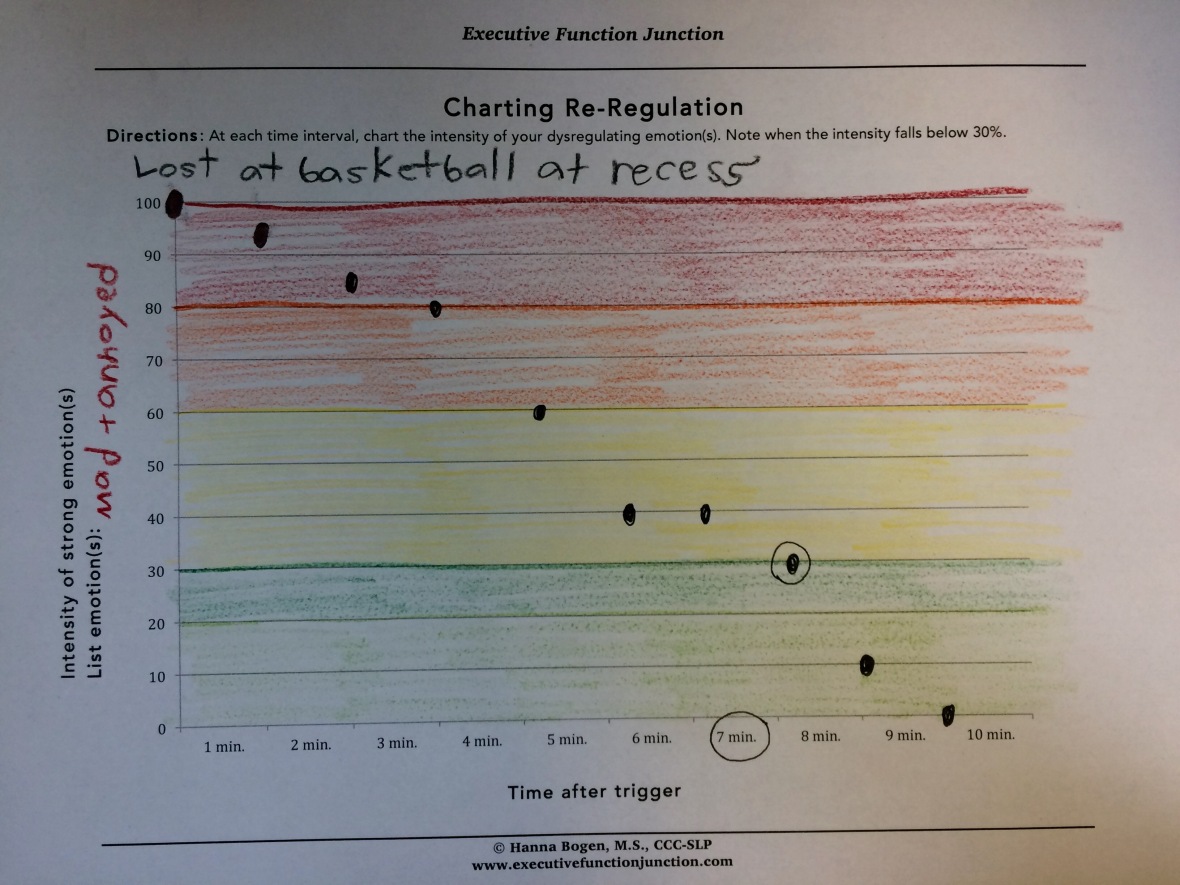
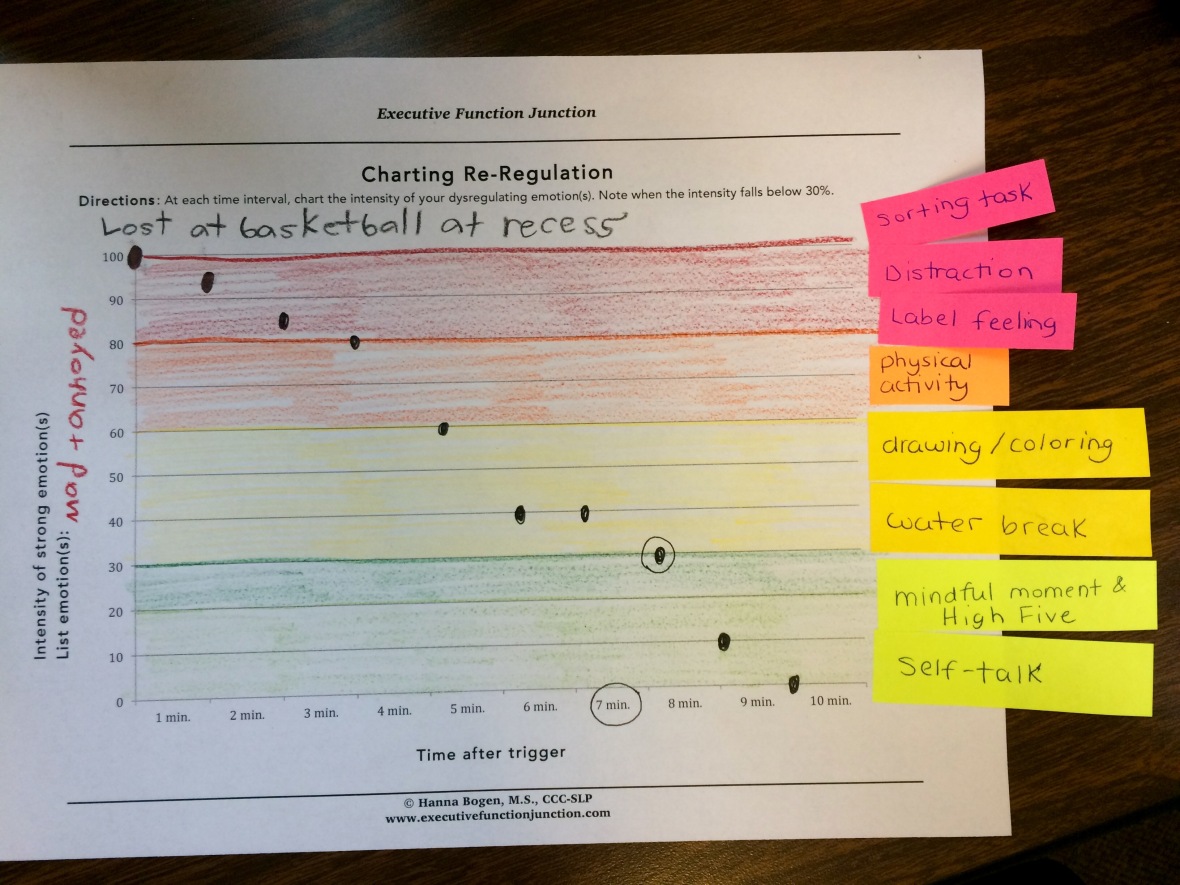
“Yes, and…”: Acknowledging and validating one’s emotionally dysregulated experience does not imply inherent agreement with that dysregulated state. As stated by the Emotional ABC’s curriculum (Venice West Productions, Inc., 2012), “emotions are like the weather.” Like the weather, we don’t strive to control our emotions; instead we strive to equip ourselves with tools and strategies to cope with the emotions that appear in various social situations. Acknowledging and validating one’s emotional experience is critical to bringing awareness to the emotional state, and providing an opportunity to engage in regulating strategies. Identifying one’s emotion(s) and moving forward to initiate a regulation strategy (i.e., “Yes, and…”) embodies the process of emotional regulation, a critical component of social-regulation (e.g., Example of self-talk: “Yes, I am feeling anxious and I can use my focus tool to calm myself.”). The social landscape is complex and dynamic, often requiring individuals to demonstrate flexibility, reciprocity, and adaptation to changing social rules. The principles of improv highlight many of the skills required for successful social experiences, and practice with improv games and activities can help to build the skills needed for social success.




 TANG YAU HOONG
TANG YAU HOONG